As a reminder, taxonomy codes are required on all claims to ensure proper claims processing and payment.
We've recently made changes to back-end matching logic for taxonomy codes, which will continuously improve the overall claim adjudication process.
Note that failure to submit claims with the applicable NPI and correct correlating taxonomy code will result in claim denials that must be corrected prior to payment consideration.
It's important that you work with your third-party billing agency and/or clearinghouse to ensure compliance with these requirements.
Review these tips for compliant billing practices related to taxonomy codes.
Claim submissions
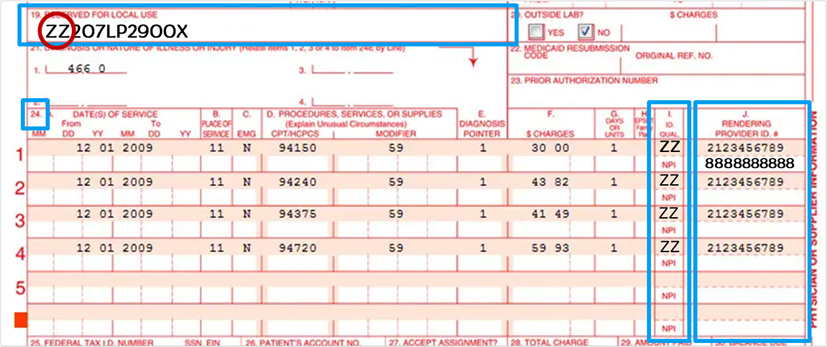
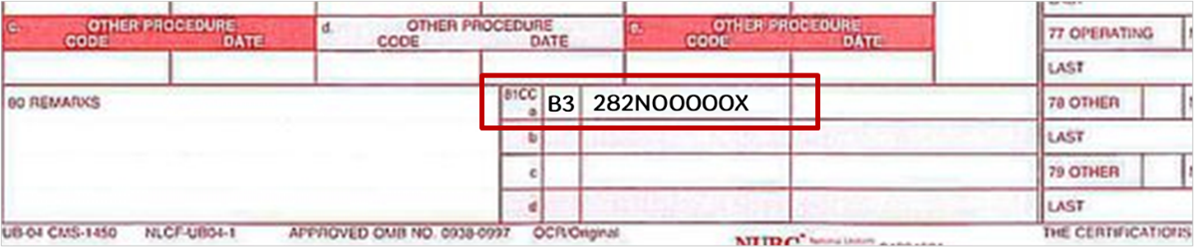
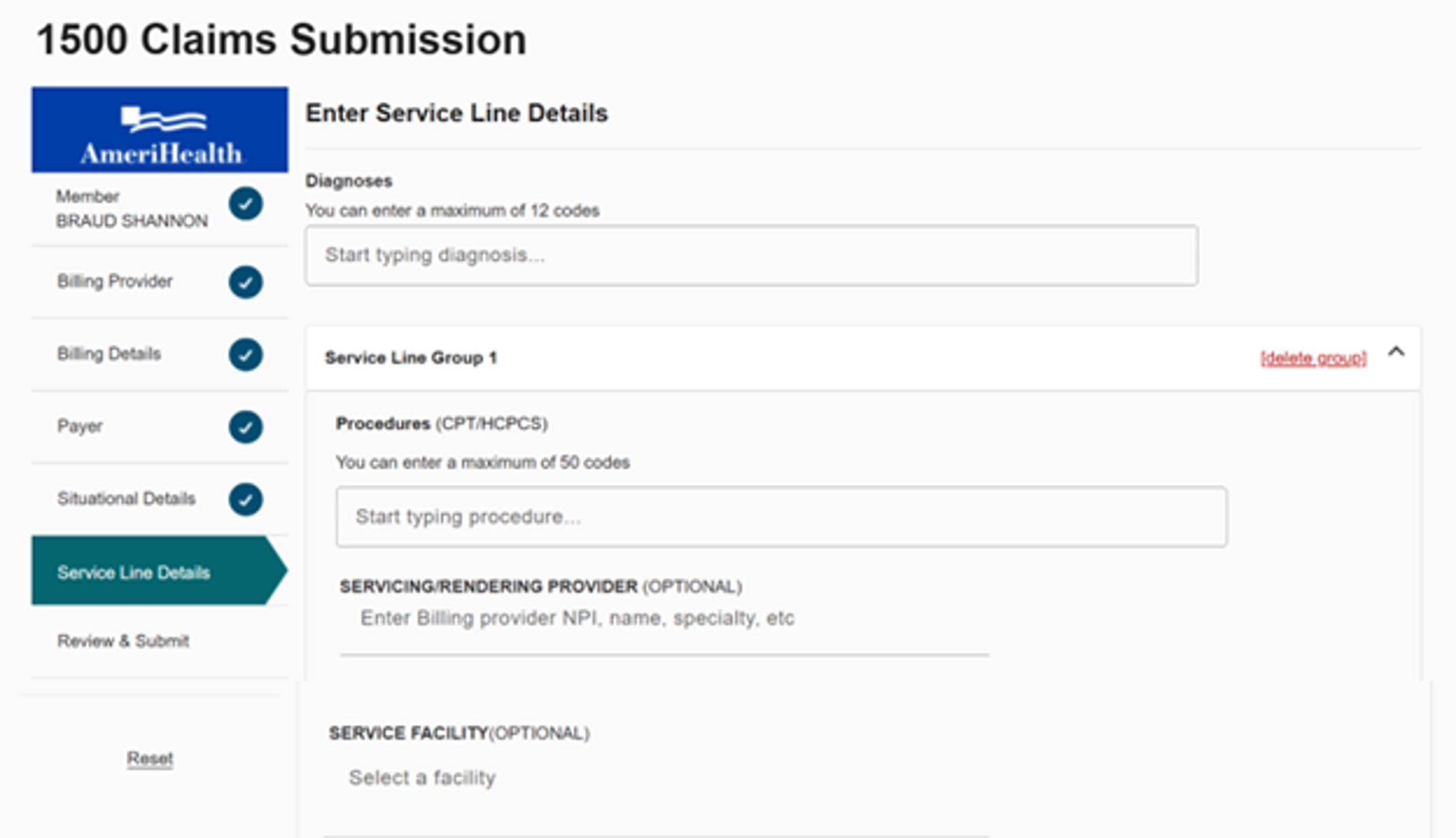
Review the visuals below for accurate
paper and
PEAR portal 1500 claim submissions:
-
CMS 1500 claim form submissions:
-
UB-04 claim form submissions:
-
PEAR Practice Management – 1500 Claim Submissions:
For guidance on
electronic
claim submissions, please review the
claim submission guides on our website.
Claim corrections
Review the visuals below to submit a corrected
paper claim.
-
CMS 1500 claim forms:
Box 22 – Resubmission and/or Original Reference Number
Follow the instructions from the National Uniform Coding Committee (NUCC) billing requirements:
-
List the original reference number for resubmitted claims.
-
When submitting a claim, enter the appropriate resubmission code in the left-hand side of the field.
-
7 = Replacement of prior claim
-
8 = Void/cancellation of prior claim
Example:

-
UB-04 claim forms:
Field location 4 – Type of Bill – Frequency Code
When submitting a claim, enter the appropriate Frequency Code in the fourth position of the Type of Bill:
-
7 = Replacement of prior claim
-
8 = Void/cancellation of prior claim
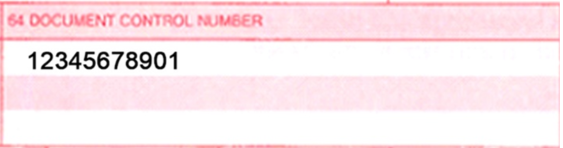
Field location 64 – Document Control Number
This field is used to capture the original reference/claim number, which is required for corrected claims.
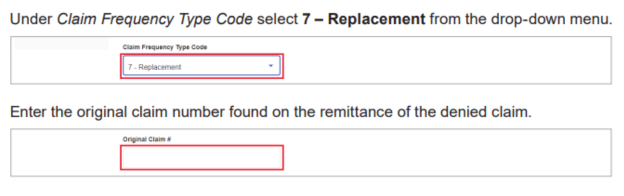
Review the visuals below from the Corrected Claims Job Aid on the PEAR Help Center for steps to submit a corrected claim in the PEAR portal.
For additional questions, please call Provider Customer Service at 1-888-YOUR
AH1 (1-888-968-7241) for New Jersey or 1-800-275-2583 for Pennsylvania. Visit
our dedicated Platform Transition page to view an
archive of communications related to the transition.
23-0201