As previously communicated, as part of our transition to a new operating platform, we will issue new ID cards to members that will display a new ID number and structure.
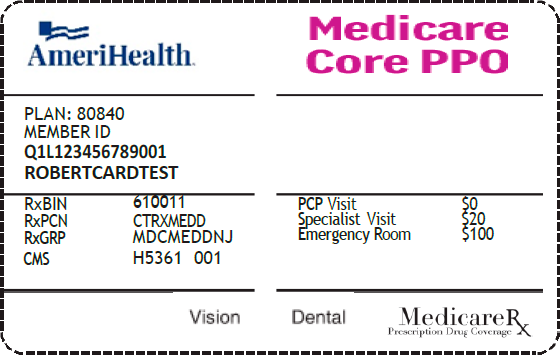
Starting January 1, 2024, as members are moved to the new platform, they will receive a new ID card with a new number structure. Members who enroll in one of the new AmeriHealth Medicare plans for 2024 will also receive an ID card with the new number structure. Below is a sample. The new ID number will be at the member level not the subscriber level, meaning each member will have a unique ID number.
New ID cards will be distributed throughout the
platform transition as a member's plan renews.
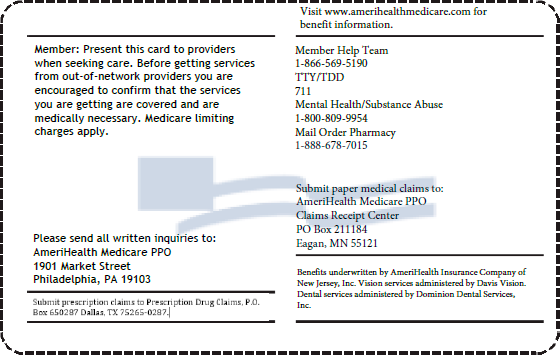
It is important to ask members for a copy of their latest ID card at every visit to ensure proper claims processing.
You can also use the Eligibility & Benefits transaction on PEAR Practice Management (PM) to confirm eligibility and view an image of the member's ID card.
Claims processing
- Claims will be processed based on the member's ID number on the date of service or date of admission. You do not need to split claims.
- Claims submitted with an old ID number after the new card is effective will be denied with this message: “Member did not have eligible coverage." If this occurs, please obtain the new ID number from the member and resubmit the claim.
- Use the updated payer ID grids for 2024 to assist with claims submission instructions. Note that the new Medicare PPO plans have been assigned a new prefix.
Stay informed
We encourage you to frequently visit our dedicated Platform Transition page to stay up to date on the upcoming changes. The FAQs are updated as new information becomes available.