Starting December 1, 2024, AmeriHealth commercial members with the National Access network will receive a new ID card when their plan renews, as part of the transition to our new operating platform.
In addition to the network indicator (e.g., AmeriHealth Advantage, Value Plus, or Regional Preferred) located on the top right of the card, the new ID cards may show one of these options, depending on the benefits purchased:
-
A Cigna PPO logo – for members with Cigna National Access
-
Both the Cigna logo and a “NY ONLY" indicator – for members with NY Access only
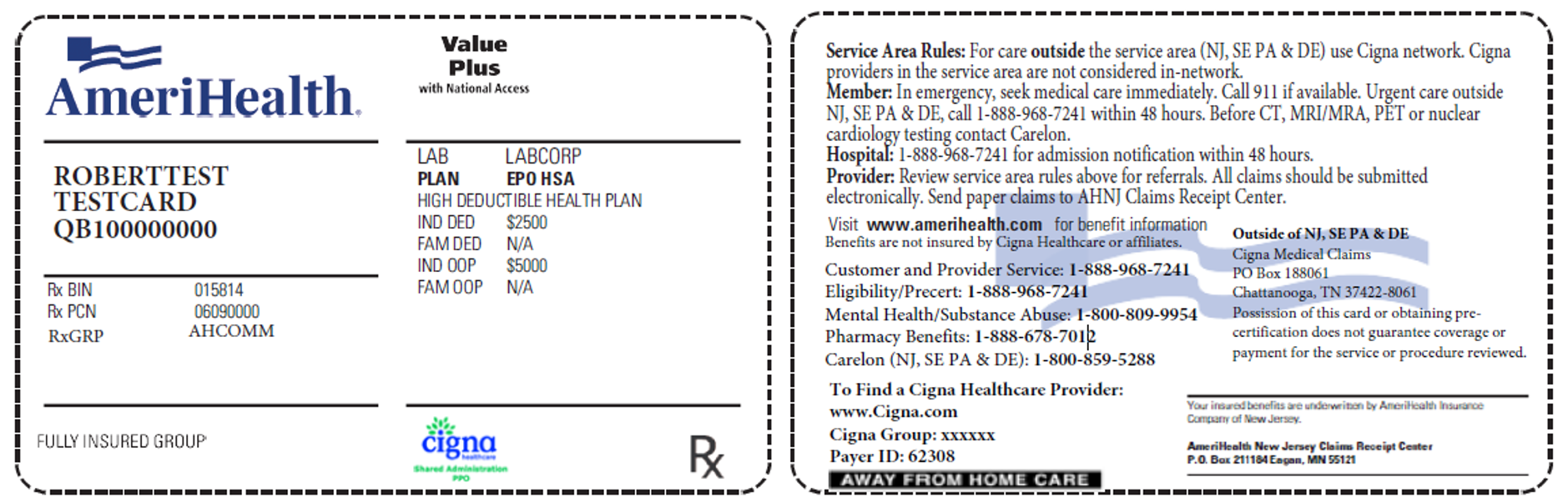
This sample represents the ID card with the Cigna logo:
This sample represents the ID card with the NY ONLY indicator:
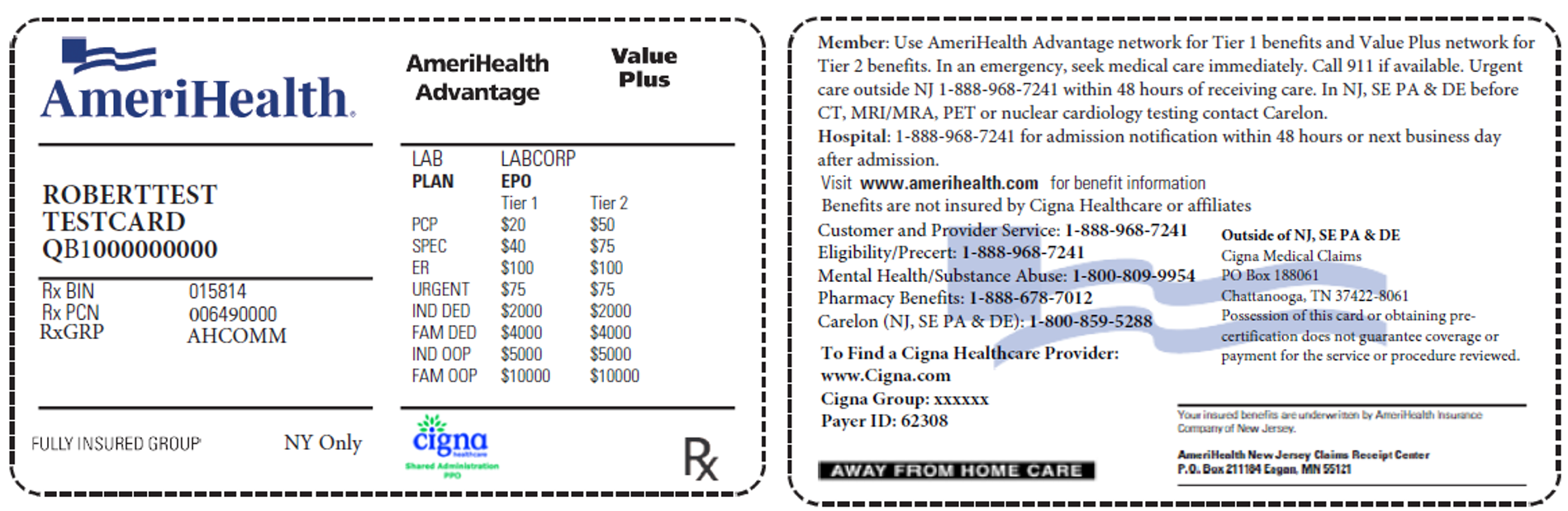
The back of the ID card will include directions for claims submissions through the Cigna network, which should only be used when a member seeks care outside of our service area (New Jersey, Delaware, and Southeastern Pennsylvania). The process for claims will differ for claims within that service area. All claims outside of New Jersey, Delaware, and Pennsylvania should be submitted directly to Cigna (payer ID: 62308). Precertification requests should also be sent to Cigna. Please don't hesitate to contact us with any questions related to the National Access network.
Note: The ID cards will also have a new member ID number, which begins after a 3-character prefix, such as QB1. Please use only the numbers that come after the 3-character prefix when corresponding with AmeriHealth.
|
New ID cards will be distributed throughout the platform transition as a member's plan renews. Therefore, it's imperative that provider offices do the following: -
Obtain a copy of the member's ID card at every visit to ensure that you submit the most up-to-date information to AmeriHealth.
-
Verify the member's plan using the Eligibility & Benefits transaction via the Practice Management application on the Provider Engagement, Analytics & Reporting (PEAR) portal.
|
Stay informed
We encourage you to frequently visit our dedicated
Platform Transition page to stay informed of upcoming changes.
24-0142